An impacted tooth refers to a tooth that fails to fully erupt through the gum into its expected position in the dental arch. This condition commonly affects wisdom teeth and can also occur with other teeth, such as canines or premolars. This blog explores the causes, symptoms, and treatment options for impacted teeth, with a focus on impacted wisdom teeth.
What is an Impacted Tooth?
An impacted tooth is one that remains stuck below the gum line or only partially erupts, unable to align properly with adjacent teeth. This condition can occur due to various factors, including overcrowding of teeth, abnormal tooth growth direction, or obstacles blocking the tooth’s path to eruption.
Types of Impacted Teeth
1. Impacted Wisdom Tooth:
Wisdom teeth, also known as third molars, commonly become impacted due to their late eruption and limited space in the jaw. Types of impacted wisdom teeth include:
– Vertical Impaction: The tooth is trapped within the jawbone, typically due to lack of space for eruption.
– Horizontal Impaction: The tooth grows horizontally against the adjacent tooth or jawbone.
– Mesial Impaction: The tooth is tilted forward, towards the front of the mouth.
– Distal Impaction: The tooth is tilted backward, towards the rear of the mouth.
2. Impacted Canine Tooth:
Canine teeth (cuspids) can also become impacted, often due to crowding or obstruction in the tooth’s path. Treatment may involve orthodontic intervention to create space or surgical exposure and traction to guide the tooth into its proper position.
Symptoms of an Impacted Tooth
Common signs and symptoms of an impacted tooth may include:
– Pain or Discomfort: Persistent pain in the jaw, gums, or adjacent teeth.
– Swelling: Swollen gums or jaw in the affected area.
– Redness and Tenderness: Inflammation and sensitivity around the impacted tooth.
– Difficulty Opening Mouth: Limited jaw movement or difficulty fully opening the mouth.
– Bad Breath: Halitosis (bad breath) due to trapped food particles and bacteria around the impacted tooth.
Diagnosis and Treatment Options
1. Dental Examination:
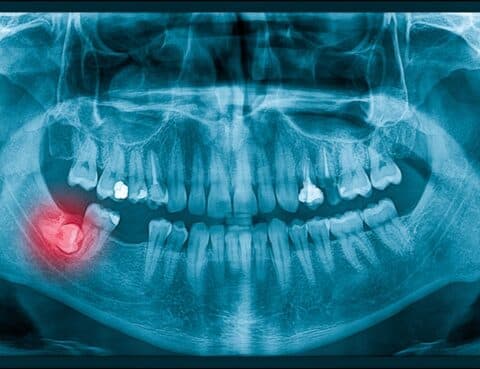
Your dentist will perform a thorough examination, which may include dental X-rays to assess the position and condition of the impacted tooth.
2. Treatment Options:
Treatment for impacted teeth depends on the tooth’s position, symptoms, and potential complications. Common treatment options include:
– Monitoring: Some impacted teeth may not require immediate treatment if they are asymptomatic and not causing problems.
– Extraction: Surgical removal of the impacted tooth may be recommended, especially if it causes pain, infection, or potential damage to adjacent teeth.
– Orthodontic Treatment: Orthodontic procedures such as braces or aligners may be used to create space and guide impacted teeth into their proper position.
– Surgical Exposure and Bonding: For impacted canines or other teeth, a surgical procedure may be performed to expose the tooth and attach an orthodontic bracket to facilitate eruption.
Impacted Wisdom Tooth Removal
1. Surgical Extraction: If a wisdom tooth is impacted or causing problems such as infection or crowding, surgical extraction may be recommended. This procedure is typically performed under local anesthesia or sedation to ensure patient comfort.
2. Post-Operative Care: After wisdom tooth removal, patients are advised to follow post-operative instructions provided by their dentist or oral surgeon. This may include taking prescribed medications, applying ice packs to reduce swelling, and sticking to a soft diet during the initial recovery period.
Conclusion
Understanding the causes, symptoms, and treatment options for impacted teeth, particularly impacted wisdom teeth, is essential for maintaining oral health and preventing complications. Regular dental check-ups and X-rays can help detect impacted teeth early, allowing for timely intervention and treatment. If you experience symptoms of an impacted tooth, consult with your dentist or oral surgeon to discuss appropriate treatment options tailored to your specific condition and oral health needs. Early diagnosis and treatment can help alleviate pain, prevent infection, and preserve overall dental health.

Experiencing tooth pain at night can be incredibly uncomfortable and disruptive to sleep. Many individuals find that their tooth pain worsens during nighttime hours, leading to throbbing sensations or even unbearable discomfort. This blog delves into the reasons behind why tooth pain intensifies at night, the common causes of nighttime tooth pain, and effective strategies to manage and alleviate this discomfort.
Understanding Nighttime Tooth Pain
1. Increased Blood Flow:
One of the primary reasons tooth pain escalates at night is due to increased blood flow to the head and face when lying down. This increased circulation can amplify sensations of pain and sensitivity in the teeth and gums, especially if there is an underlying dental issue.
2. Changes in Posture:
When you lie down to sleep, changes in posture can affect how blood flows to your head and face. This change in blood flow can lead to increased pressure in the nerves surrounding your teeth, making any existing dental pain more noticeable.
3. Sinus Congestion:
Sinus congestion or infections can also contribute to nighttime tooth pain. The sinuses are located close to the upper teeth, and pressure from sinus inflammation can radiate to the teeth, exacerbating pain, especially when lying down.
4. Bruxism (Teeth Grinding):
Bruxism, a condition where individuals grind or clench their teeth involuntarily during sleep, can lead to excessive pressure on the teeth and jaws. This pressure can cause tooth sensitivity and pain, which is often worse at night.
5. Temperature Changes:
Drinking hot or cold beverages before bed can trigger tooth sensitivity and pain, particularly in teeth with exposed nerves or dental work. The contrast in temperature can cause the tooth’s nerve endings to react, leading to discomfort.
Common Causes of Nighttime Tooth Pain
1. Tooth Decay:
Decayed teeth with cavities can expose the tooth’s sensitive inner layers (dentin) to stimuli such as temperature changes or pressure, resulting in pain that may worsen at night.
2. Dental Abscess:
A dental abscess is a severe infection at the root of a tooth or between the tooth and gums. The buildup of pus and pressure can cause throbbing, intense pain, particularly when lying down.
3. Gum Disease:
Gum disease, such as gingivitis or periodontitis, can lead to inflammation and infection of the gums. This can cause gums to recede, exposing tooth roots and increasing sensitivity and pain, especially at night.
4. Tooth Fractures or Cracks:
Fractured or cracked teeth can cause intermittent or constant pain, which may worsen at night when lying down due to changes in blood flow and pressure.
Managing Nighttime Tooth Pain
1. Pain Relief Medications:
Over-the-counter pain relievers such as ibuprofen or acetaminophen can provide temporary relief from nighttime tooth pain. Follow dosage instructions and consult with a dentist if pain persists.
2. Oral Hygiene Practices:
Maintain good oral hygiene habits, including brushing twice daily and flossing, to prevent tooth decay and gum disease that can contribute to nighttime tooth pain.
3. Avoiding Triggers:
Limit consumption of sugary foods and beverages, acidic foods, and extreme temperatures that can aggravate tooth sensitivity and pain.
4. Dental Consultation:
Schedule an appointment with your dentist if you experience persistent or severe nighttime tooth pain. They can perform a thorough examination, including X-rays if needed, to diagnose the underlying cause and recommend appropriate treatment.
Conclusion
Nighttime tooth pain can stem from various causes, including dental issues like decay, abscesses, or gum disease, as well as external factors like bruxism or sinus problems. Understanding these causes and implementing effective management strategies, such as pain relief medications, oral hygiene practices, and dental treatments, can help alleviate nighttime tooth pain and promote overall oral health. Regular dental check-ups and prompt treatment of dental problems are essential for preventing recurring tooth pain and maintaining a healthy smile. If nighttime tooth pain persists despite home care efforts, seek professional dental advice for a personalized treatment plan to address the underlying cause of your discomfort.

Tooth extraction is a common dental procedure performed for various reasons, from severe decay to overcrowding. This blog explores the process of tooth extraction, including timelines for recovery, potential complications like infection, and considerations for subsequent dental implants.
Process of Tooth Extraction
1. Initial Assessment:
Before performing a tooth extraction, your dentist will conduct a thorough examination of the affected tooth and surrounding oral structures. This may involve X-rays to assess the tooth’s position and root structure.
2. Anesthesia and Extraction:
On the day of the extraction, local anesthesia is administered to numb the area around the tooth. For complex cases or multiple extractions, general anesthesia may be used. The dentist then carefully loosens the tooth using specialized instruments and extracts it from the socket.
3. Post-Extraction Care:
After the tooth is removed, gauze is placed over the extraction site to control bleeding. Your dentist may provide instructions on how to manage pain and swelling, as well as recommend over-the-counter pain relievers if needed.
Timeline for Recovery
1. Immediate Aftercare:
The initial healing period involves blood clot formation at the extraction site, which is crucial for proper healing. Avoiding vigorous rinsing, spitting, or drinking through a straw helps prevent dislodging the clot.
2. First Few Days:
Mild to moderate discomfort and swelling are common in the first few days after extraction. Applying ice packs to the outside of the face and following prescribed pain medications can help manage these symptoms.
3. Week 1-2:
During this period, the extraction site begins to heal. New tissue forms, and any residual discomfort typically subsides. It’s essential to maintain good oral hygiene by gently brushing the teeth near the extraction site and rinsing with saltwater as instructed.
Complications and Considerations
1. Infection:
While uncommon, infection after tooth extraction can occur if the extraction site is not kept clean or if there are underlying health conditions. Signs of infection include persistent pain, swelling, fever, or foul-smelling discharge. Prompt dental evaluation and antibiotic treatment may be necessary if infection occurs.
2. Dry Socket:
Dry socket is a painful condition that can develop when the blood clot is dislodged or fails to form properly after extraction. This exposes the underlying bone and nerves, causing intense pain. Your dentist can provide treatments such as medicated dressings to alleviate symptoms and promote healing.
Tooth Extraction and Implant Timeline
1. Healing Period:
The duration of healing after tooth extraction varies depending on factors such as the location of the tooth, patient’s overall health, and adherence to post-operative care instructions. Most extraction sites heal within a few weeks.
2. Implant Consideration:
If a dental implant is planned to replace the extracted tooth, your dentist may recommend waiting for the extraction site to fully heal before proceeding with implant placement. This ensures optimal bone integration and reduces the risk of complications.
Conclusion
Tooth extraction is a routine dental procedure aimed at alleviating pain, preventing infection, and improving overall oral health. Understanding the process, timeline for recovery, and potential complications such as infection or dry socket can help patients prepare for the procedure and manage expectations post-operatively. Following your dentist’s instructions for aftercare, maintaining good oral hygiene, and seeking prompt dental attention if complications arise are essential steps towards a smooth recovery and successful treatment outcomes. If you’re considering tooth extraction or have concerns about your oral health, consult with your dentist to discuss personalized treatment options and ensure comprehensive care.

Tooth decay, also known as dental caries or cavities, is a common oral health issue caused by bacteria that gradually erode tooth enamel. This blog explores the causes of tooth decay, its symptoms, stages, treatment options, and effective preventive measures.
Causes of Tooth Decay
Tooth decay occurs when acids produced by bacteria in plaque attack the tooth enamel. The following factors contribute to the development of dental caries:
1. Poor Oral Hygiene:
Incomplete removal of plaque through brushing and flossing allows bacteria to thrive on teeth, leading to enamel erosion and decay.
2. Diet High in Sugars and Starches:
Frequent consumption of sugary foods and beverages provides fuel for bacteria to produce acids that attack tooth enamel. Starchy foods can also break down into sugars, contributing to decay.
3. Acidic Foods and Drinks:
Acidic foods and beverages (e.g., citrus fruits, soda) can weaken enamel, making it more susceptible to decay.
4. Dry Mouth:
Saliva plays a crucial role in neutralizing acids and washing away food particles. Reduced saliva production, often caused by medical conditions or medications, can increase the risk of tooth decay.
5. Dental Plaque and Tartar:
Plaque that isn’t removed can harden into tartar (calculus), which harbors bacteria and accelerates enamel erosion.
Symptoms of Tooth Decay
Early stages of tooth decay may not cause noticeable symptoms. As decay progresses, symptoms can include:
– Tooth Sensitivity: Sensitivity to hot, cold, sweet, or acidic foods and beverages.
– Toothache: Spontaneous pain or discomfort in a tooth.
– Visible Holes or Pits: Dark spots or visible holes (cavities) on the tooth surface.
– Bad Breath: Persistent bad breath (halitosis) despite oral hygiene efforts.
Stages of Tooth Decay
1. Enamel Decay:
Initial stage characterized by demineralization of tooth enamel. At this stage, decay can often be reversed with fluoride treatments and improved oral hygiene.
2. Dentin Decay:
As decay progresses, bacteria penetrate deeper into the tooth, reaching the softer dentin layer beneath the enamel. This stage may cause increased sensitivity and pain.
3. Pulp Involvement:
Advanced decay reaches the innermost layer of the tooth (pulp), containing nerves and blood vessels. Severe pain, infection (abscess), and potential tooth loss can occur without prompt treatment.
Treatment Options for Tooth Decay
1. Fluoride Treatment:*
In early stages, fluoride treatments can remineralize weakened enamel and halt the progression of decay.
2. Dental Fillings:
For cavities, dentists remove decayed portions of the tooth and fill the cavity with materials such as composite resin, amalgam, or porcelain to restore its shape and function.
3. Root Canal Therapy:
If decay reaches the tooth’s pulp, root canal therapy may be necessary to remove infected tissue, disinfect the root canal, and seal it with a filling or crown.
4. Dental Crowns or Inlays/Onlays:
For extensive decay or weakened teeth, crowns or inlays/onlays may be placed to restore strength and protect the tooth.
5. Tooth Extraction:
In cases of severe decay or infection where restoration is not feasible, the tooth may need to be extracted.
Preventive Measures to Stop Tooth Decay
1. Maintain Good Oral Hygiene:
Brush twice daily with fluoride toothpaste, floss daily, and use an antimicrobial mouthwash to remove plaque and bacteria.
2. Balanced Diet:
Limit sugary and acidic foods and beverages. Choose nutritious foods that support oral health, such as fruits, vegetables, and dairy products.
3. Regular Dental Visits:
Schedule regular dental check-ups and cleanings to detect and treat early signs of decay before they progress.
4. Fluoride Supplements:
For individuals at higher risk of decay, fluoride supplements may be recommended by a dentist or healthcare provider.
Conclusion
Tooth decay is a preventable condition that can lead to pain, infection, and tooth loss if left untreated. By understanding the causes, recognizing symptoms, and adopting effective preventive measures such as good oral hygiene, balanced diet, and regular dental care, individuals can maintain optimal oral health and reduce the risk of dental caries. Early detection and timely treatment of tooth decay are essential for preserving natural teeth and preventing complications. If you experience symptoms of tooth decay or have concerns about your oral health, consult with your dentist for personalized advice and treatment options tailored to your needs.

Do you find yourself unconsciously clenching your jaw throughout the day? If so, you may be experiencing a condition known as bruxism, which involves grinding or clenching your teeth, often without realizing it. Not only can this habit lead to dental issues, but it can also cause headaches and jaw pain. In this blog, we’ll delve into the causes of unconsciously clenching jaw, explore the effects it can have on your health, and discuss practical strategies to help you kick this habit to the curb.
Understanding Unconsciously Clenching Jaw:
Unconsciously clenching jaw, or bruxism, is a common condition that affects many individuals. While some people may experience bruxism primarily during sleep, others may clench their jaw involuntarily during the day as well. Stress and anxiety are often major contributors to jaw clenching, as tension in the jaw muscles can build up as a result of emotional stressors. Additionally, misalignment of the teeth or temporomandibular joint (TMJ) can also play a role in bruxism.
The Effects of Unconsciously Clenching Jaw:
Unconsciously clenching jaw can have various negative effects on your oral health and overall well-being. Continuous clenching and grinding of the teeth can wear down the enamel, leading to tooth sensitivity, fractures, and even tooth loss in severe cases. Furthermore, the constant strain on the jaw muscles can result in jaw pain, headaches, and temporomandibular joint disorders (TMD), causing discomfort and reducing quality of life.
Practical Strategies to Stop Unconsciously Clenching Jaw:
If you’re struggling with unconsciously clenching jaw, there are several strategies you can implement to help break this habit and alleviate associated symptoms:
1. Stress Management Techniques: Since stress is a major trigger for jaw clenching, learning effective stress management techniques can help reduce tension in the jaw muscles. Practice relaxation techniques such as deep breathing, meditation, yoga, or tai chi to promote relaxation and alleviate stress.
2. Jaw Muscle Exercises: Performing specific exercises to strengthen and relax the jaw muscles can help reduce unconscious clenching. Simple exercises such as gently massaging the jaw muscles, opening and closing the mouth slowly, and stretching the jaw muscles can promote relaxation and alleviate tension.
3. Behavioral Therapy: Cognitive-behavioral therapy (CBT) can be beneficial for addressing the underlying causes of bruxism, such as stress and anxiety. A therapist can help you identify triggers for jaw clenching and develop coping strategies to manage stress more effectively.
4. Use of Mouthguards: Wearing a custom-fitted mouthguard or splint at night can help protect your teeth from the effects of grinding and clenching while you sleep. Additionally, wearing a daytime mouthguard can prevent unconsciously clenching jaw during the day and reduce associated symptoms.
5. Dental Treatments: In some cases, dental treatments such as orthodontic adjustments or dental restorations may be necessary to correct misalignment issues that contribute to bruxism. Consult your dentist to determine the most appropriate treatment options for your specific needs.
6. Lifestyle Modifications: Adopting healthy lifestyle habits such as maintaining good posture, avoiding excessive caffeine and alcohol consumption, and getting an adequate amount of sleep can help reduce stress and promote overall relaxation, thereby decreasing the likelihood of jaw clenching.
In conclusion, unconsciously clenching jaw can have detrimental effects on your oral health and well-being, but it’s not something you have to endure. By implementing effective strategies such as stress management techniques, jaw muscle exercises, and the use of mouthguards, you can take control of your jaw clenching habit and alleviate associated symptoms. Remember to consult your dentist or healthcare provider for personalized advice and treatment options tailored to your needs. With dedication and persistence, you can say goodbye to jaw clenching and hello to a healthier, more relaxed jaw.

Are yellow teeth causing you to hide your smile? You’re not alone. Many individuals experience discoloration in their teeth at some point in their lives. But fear not, there are numerous strategies to combat this issue and restore the brightness to your smile. In this blog, we’ll delve into the causes of yellow teeth, dispel common myths, and explore effective methods to regain your pearly whites.
Understanding Yellow Teeth:
Firstly, it’s essential to understand that teeth naturally vary in shade. While some people have naturally whiter teeth, others have teeth that are naturally more yellowish. Factors such as genetics, age, and lifestyle habits can influence the color of your teeth. However, even if your teeth are naturally yellow, there are still steps you can take to enhance their appearance.
Common Causes of Yellow Teeth:
Several factors contribute to teeth turning yellow. One of the primary culprits is poor oral hygiene. Inadequate brushing and flossing allow plaque and tartar to accumulate, leading to surface stains and yellowing. Additionally, certain foods and beverages such as coffee, tea, red wine, and dark-colored berries contain pigments that can stain teeth over time. Smoking and tobacco use are also major contributors to yellow teeth due to the tar and nicotine present in cigarettes. Moreover, some medical conditions and medications can cause tooth discoloration.
Debunking Myths:
Before diving into remedies, let’s address some common myths surrounding yellow teeth. Contrary to popular belief, yellow teeth are not necessarily stronger than white teeth. The color of your teeth is primarily determined by the enamel, the outer layer of the tooth. While enamel varies in thickness among individuals, yellow teeth are not inherently healthier or stronger than white teeth. Additionally, vaping, although often considered a safer alternative to smoking, can still contribute to tooth discoloration. The aerosol from vaping contains chemicals that can stain teeth over time.
Effective Strategies for Whiter Teeth:
Now that we’ve debunked some myths, let’s explore practical ways to whiten yellow teeth:
1. Maintain Good Oral Hygiene: Brush your teeth at least twice a day and floss daily to remove plaque and prevent stains from forming.
2. Limit Stain-Causing Foods and Beverages: Reduce your consumption of coffee, tea, wine, and other foods that can stain teeth. When consuming them, rinse your mouth with water afterward to minimize staining.
3. Quit Smoking and Tobacco Use: By quitting smoking and other tobacco products, you can prevent further yellowing of your teeth and improve your overall oral health.
4. Professional Teeth Whitening: Consider professional teeth whitening treatments offered by dentists. These treatments use bleaching agents to effectively lighten the color of your teeth.
5. Over-the-Counter Whitening Products: There are numerous over-the-counter whitening products available, such as whitening toothpaste, strips, and gels. While these products may not be as effective as professional treatments, they can still help reduce surface stains and improve the appearance of your teeth.
6. Regular Dental Check-ups: Visit your dentist regularly for professional cleanings and check-ups. Your dentist can identify any underlying issues contributing to yellowing teeth and recommend appropriate treatments.
In conclusion, yellow teeth are a common concern, but they’re not something you have to live with. By understanding the causes of yellow teeth and adopting good oral hygiene habits, you can effectively combat tooth discoloration and achieve a brighter, more confident smile. Remember, consistency is key, so stick to your oral care routine and consult your dentist for personalized advice and treatment options. With dedication and proper care, you can say goodbye to yellow teeth and hello to a dazzling smile.

A dental fistula, also known as a gum fistula or fistula on gums, is a small tunnel that forms between an infected tooth and the surrounding gum tissue or skin. While it may appear as a small bump or pimple on the gums, a dental fistula is often a sign of an underlying dental infection that requires prompt attention. Let’s explore the causes, symptoms, and treatment options for fistulas on gums to help you better understand this oral health condition.
What Causes Fistulas on Gums?
Dental fistulas typically develop as a result of a dental abscess, which is a pocket of pus caused by a bacterial infection in the tooth or surrounding gum tissue. The infection may originate from untreated tooth decay, a cracked or fractured tooth, or advanced gum disease. As the infection progresses, pressure builds up within the tooth, leading to the formation of a fistula as the body attempts to release the trapped pus and bacteria.
Symptoms of Fistulas on Gums:
The most common symptom of a dental fistula is the presence of a small bump or pimple on the gums near the affected tooth. Other symptoms may include:
– Persistent or throbbing toothache
– Swelling and tenderness in the gums
– Redness or inflammation around the affected area
– Pus or discharge draining from the fistula
– Foul taste or odor in the mouth
– Fever or general feelings of illness in severe cases
If you experience any of these symptoms, it’s essential to seek dental care promptly to prevent the spread of infection and potential complications.
Treatment Options for Fistulas on Gums:
The treatment for a dental fistula typically involves addressing the underlying dental infection and restoring oral health. Depending on the severity of the infection and the extent of damage to the tooth and surrounding tissues, treatment options may include:
– Root Canal Therapy: If the infection is confined to the pulp chamber and root canals of the affected tooth, root canal therapy may be recommended. During this procedure, the infected pulp is removed, and the tooth is thoroughly cleaned and sealed to prevent further infection.
– Drainage: In cases where the dental abscess has already formed a fistula, your dentist may need to drain the pus and fluid from the fistula to relieve pressure and facilitate healing. This may be done through a small incision in the gum tissue or by enlarging the existing fistula opening.
– Antibiotic Therapy: Antibiotics may be prescribed to help control the spread of infection and reduce inflammation. However, antibiotics alone are not sufficient to treat a dental abscess and should be used in conjunction with other dental treatments.
– Tooth Extraction: In severe cases where the tooth is extensively damaged or the infection cannot be effectively treated with root canal therapy, extraction of the affected tooth may be necessary to prevent further complications.
Preventive Measures:
To reduce the risk of developing a dental fistula and other oral health problems, it’s essential to practice good oral hygiene habits, including:
– Brushing your teeth twice daily with fluoride toothpaste
– Flossing between your teeth daily to remove plaque and debris
– Visiting your dentist regularly for check-ups and professional cleanings
– Avoiding sugary foods and beverages that can contribute to tooth decay
– Seeking prompt dental care for any signs of toothache, swelling, or gum irritation
By taking proactive steps to maintain your oral health, you can help prevent the development of dental fistulas and other potentially serious dental conditions.
In conclusion, a dental fistula on the gums is a visible sign of an underlying dental infection that requires prompt attention from a dentist. By recognizing the symptoms and seeking timely treatment, you can prevent further complications and restore oral health. If you suspect you may have a dental fistula or are experiencing any symptoms of a dental infection, don’t hesitate to schedule an appointment with your dentist for evaluation and treatment.

Have you ever run your tongue along your teeth and felt a sudden, sharp sensation? If so, you’re not alone. Many people experience the discomfort of sharp teeth, leaving them wondering: why do my teeth feel sharp on my tongue? Let’s delve into the potential causes of this phenomenon and explore how to address sharp teeth for a smoother, more comfortable oral experience.
1. Wear and Tear:
One of the most common reasons for teeth feeling sharp is wear and tear over time. As we age, the enamel, the protective outer layer of the teeth, can gradually wear down due to factors such as chewing, grinding, or brushing too vigorously. When the enamel wears away, the underlying dentin, which is softer and more sensitive, may become exposed, leading to rough or jagged edges on the teeth that can feel sharp against the tongue.
2. Tooth Fractures or Chips:
Accidents, trauma, or biting down on hard objects can result in tooth fractures or chips, causing irregularities in the tooth’s surface that may feel sharp to the touch. Even minor chips or cracks can create rough edges that irritate the tongue or cheeks, leading to discomfort or pain. If you suspect a tooth fracture or chip, it’s essential to consult with your dentist promptly to prevent further damage and address the issue.
3. Dental Restorations:
Dental restorations such as fillings, crowns, or veneers can sometimes result in sharp edges or rough surfaces if not properly shaped or polished. Additionally, as dental restorations age, they may wear down or become damaged, leading to irregularities that can feel sharp against the tongue. Regular dental check-ups and maintenance can help ensure that your dental restorations remain smooth and comfortable.
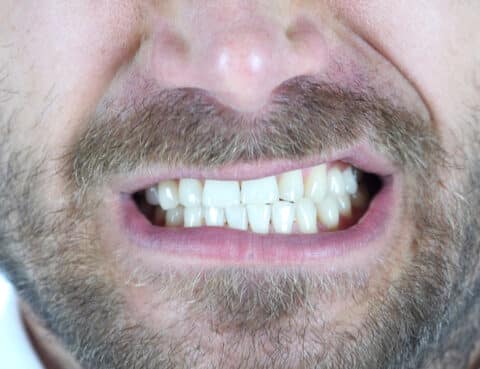
4. Misaligned Teeth:
Teeth that are misaligned or crooked can create areas of overlap or protrusion that may feel sharp against the tongue or cheeks. Misaligned teeth can result from genetics, crowded teeth, or habits such as thumb sucking or tongue thrusting. Orthodontic treatment, such as braces or clear aligners, can help correct misalignment issues and create a smoother, more comfortable bite.
5. How to Address Sharp Teeth:
If you’re experiencing discomfort or irritation due to sharp teeth, there are several steps you can take to address the issue:
– Visit Your Dentist: Schedule a dental appointment to have your teeth examined by a professional. Your dentist can identify the underlying cause of the sharpness and recommend appropriate treatment, such as filing down rough edges or repairing damaged teeth.
– Practice Good Oral Hygiene: Maintaining a consistent oral hygiene routine, including brushing twice daily, flossing, and using a fluoride mouthwash, can help prevent enamel erosion and reduce the risk of sharp teeth.
– Avoid Habits that Contribute to Wear and Tear: Be mindful of habits such as teeth grinding, nail biting, or chewing on hard objects, as these can contribute to tooth wear and exacerbate sharpness.
– Consider Orthodontic Treatment: If misaligned teeth are the culprit behind sharp sensations, orthodontic treatment may be necessary to correct the alignment and create a more comfortable bite.
In conclusion, sharp teeth sensations can result from various factors, including wear and tear, dental damage, or misalignment. By identifying the underlying cause and taking proactive steps to address it, you can enjoy a smoother, more comfortable oral experience and maintain optimal dental health for years to come.

For years, the prevailing wisdom in dentistry was to remove wisdom teeth as a precautionary measure to prevent potential problems down the line. However, recent research and evolving dental practices have led experts to reconsider this approach. Contrary to popular belief, there are several benefits to keeping your wisdom teeth when they are healthy and properly aligned. Let’s explore why experts now advocate for retaining these third molars and whether you should consider keeping yours.
1. Proper Alignment and Functionality:
One of the primary reasons experts now advise against routine wisdom teeth removal is that not all wisdom teeth pose a risk of complications. In cases where the wisdom teeth erupt fully, align properly with the adjacent teeth, and function without causing discomfort or difficulty in cleaning, there may be no need for extraction. These properly aligned wisdom teeth can contribute to the overall function of your bite and chewing ability, supporting optimal oral health.
2. Dental Stability:
Wisdom teeth, when healthy and well-positioned, can provide essential support to the adjacent teeth and help maintain dental stability. By occupying space at the back of the mouth, wisdom teeth can prevent neighboring teeth from shifting or drifting out of alignment over time. This can help preserve the integrity of your dental arch and reduce the risk of overcrowding or misalignment, which may necessitate orthodontic treatment in the future.
3. Potential Future Need:
While wisdom teeth may not serve a significant purpose in modern diets and jaw sizes, there is emerging evidence suggesting that they may have potential benefits in the event of tooth loss later in life. In some cases, wisdom teeth can serve as a source of replacement teeth if other molars are lost due to decay, trauma, or other dental issues. By retaining your wisdom teeth, you may preserve this potential resource for future dental needs.
4. Avoiding Surgical Risks:
Wisdom tooth extraction is a surgical procedure that carries inherent risks, including infection, nerve damage, and prolonged recovery time. By opting to keep your wisdom teeth when they are healthy and pose no immediate risk, you can avoid the potential complications associated with surgery and the inconvenience of downtime for recovery. This approach aligns with the principles of minimally invasive dentistry and prioritizes preserving natural teeth whenever possible.
5. Personalized Dental Care:
Ultimately, the decision to keep or remove wisdom teeth should be based on individual factors, including the specific characteristics of your teeth, your overall oral health, and your dentist’s recommendations. A thorough examination and consultation with your dentist can help determine whether your wisdom teeth are likely to cause problems in the future and whether extraction is necessary for your oral health and well-being.
In conclusion, while wisdom teeth removal has long been considered a standard practice in dentistry, experts now recognize that it may not be necessary or beneficial for everyone. Retaining healthy wisdom teeth that are properly aligned and functional can contribute to dental stability, function, and potentially serve as a resource for future dental needs. However, each case is unique, and it’s essential to consult with your dentist to determine the best course of action for your individual oral health needs.
If you’ve ever experienced the discomfort of teeth and gums hurting when you’re sick, you’re not alone. Many people report increased dental sensitivity or pain during illness, leaving them wondering: why do my teeth hurt when I’m sick? Let’s explore some of the common reasons behind this phenomenon and what you can do to alleviate the discomfort.
1. Sinus Congestion:
One of the primary reasons your teeth may hurt when you’re sick is sinus congestion. During illness, particularly colds or sinus infections, the sinuses can become inflamed and congested, putting pressure on the surrounding structures, including the teeth. This pressure can cause discomfort or pain, particularly in the upper teeth, as they are situated close to the sinus cavities.
2. Tooth Grinding:
Stress and discomfort associated with being sick can lead to unconscious habits such as tooth grinding or clenching, especially during sleep. This excessive pressure on the teeth can result in tooth sensitivity or soreness, particularly in the lower teeth and jaw area. If you notice increased tooth pain during illness, it’s essential to be mindful of any teeth grinding habits and consider using a mouthguard to protect your teeth.
3. Dehydration:
Dehydration is a common side effect of illness, as fever, sweating, and decreased fluid intake can lead to a loss of hydration in the body. When your body is dehydrated, your mouth may produce less saliva, which plays a crucial role in protecting the teeth and gums from bacteria and acid. Without an adequate saliva flow, the teeth may become more susceptible to sensitivity or discomfort, especially when consuming hot or cold foods and beverages.
4. Acid Reflux:
Some illnesses, particularly gastrointestinal conditions like acid reflux or gastroesophageal reflux disease (GERD), can lead to the reflux of stomach acid into the mouth. This acid exposure can erode the enamel, the protective outer layer of the teeth, leading to increased tooth sensitivity or pain. If you experience frequent acid reflux during illness, it’s essential to manage the condition with lifestyle changes or medications prescribed by your healthcare provider to protect your dental health.
5. Infection or Inflammation:
In some cases, dental pain during illness may be indicative of an underlying dental issue, such as a dental infection or inflammation. Illness can weaken the body’s immune response, making it more susceptible to oral infections or exacerbating existing dental problems. If you experience severe or persistent tooth pain during illness, it’s crucial to consult with your dentist to rule out any underlying dental issues and receive appropriate treatment.
Conclusion:
While experiencing tooth pain or sensitivity during illness can be uncomfortable, it’s often a temporary side effect that resolves once the underlying illness has passed. However, if you experience severe or persistent dental pain, it’s essential to seek professional dental care to address any underlying issues and prevent further complications.
In the meantime, practicing good oral hygiene, staying hydrated, managing stress, and addressing any underlying health conditions can help alleviate tooth pain and promote overall dental health, even during illness.
